Reading time: 11 minutes
Why Trauma Treatment Is Evolving
For many people, trauma is not something they remember.
It is something their body keeps repeating.
Trauma is one of the most common and least understood drivers of long-term mental suffering. For many people, trauma does not stay in the past. It continues to shape thoughts, emotions, behavior, and the body’s stress response long after the original event has ended. Trauma often intersects with broader mental health conditions such as anxiety, depression, and grief
Conventional treatments such as psychotherapy and medication help many individuals. Yet a significant group continues to struggle with persistent symptoms, emotional numbness, hypervigilance, or recurring intrusive memories. For them, progress can feel slow, incomplete, or fragile.
Over the past decade, interest has grown in psychedelic-assisted approaches, including psilocybin. This interest is not driven by trends or hype alone. It reflects deeper questions within psychiatry and neuroscience about how trauma is stored, processed, and potentially healed.
To understand why psilocybin is being studied for trauma, we first need to understand what trauma really is.
What Is Trauma?
Trauma is not defined by the event itself, but by how the nervous system responds to overwhelming stress. When an experience exceeds a person’s capacity to cope, the brain and body may shift into survival mode.
Post-traumatic stress disorder, or PTSD, is one clinical outcome of trauma. It can include symptoms such as intrusive memories, avoidance, emotional numbing, sleep disturbances, and heightened reactivity. Complex trauma often develops after repeated or prolonged exposure to stress, such as childhood neglect, abuse, or long-term relational trauma.
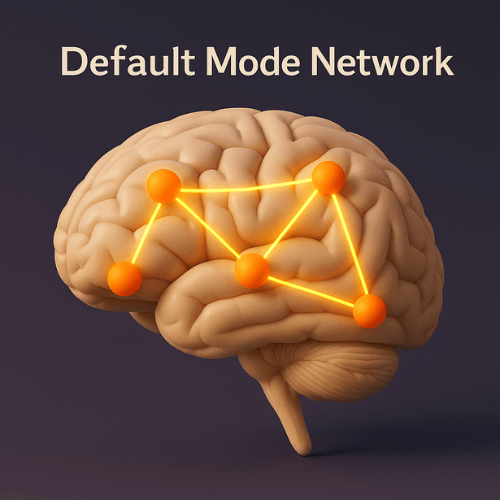
From a neurobiological perspective, trauma affects multiple brain systems. The amygdala, which detects threat, becomes more reactive. The hippocampus, involved in memory and context, may struggle to properly integrate traumatic experiences. The default mode network, which supports self-referential thinking, can become rigid and dominated by fear-based narratives.
This is why trauma is not simply a memory problem. It is a pattern of nervous system activation that continues to operate as if danger is still present, even when it is not.
Complex trauma often develops after repeated or prolonged exposure to stress, such as childhood neglect, abuse, or long-term relational trauma.
Types of Trauma
Trauma can take many forms, and not all trauma presents in the same way.
- Acute trauma results from a single overwhelming event, such as an accident or assault.
- Chronic trauma develops through repeated exposure to stress, often without recovery time in between.
- Developmental trauma occurs early in life, when the brain and nervous system are still forming.
- Relational trauma arises from attachment disruptions, emotional neglect, or unstable caregiving.
Current research suggests that psilocybin-assisted approaches may be more relevant for certain trauma profiles than others. Trauma linked to emotional avoidance, rigid fear responses, or deeply internalized beliefs about safety and self-worth appears more responsive than trauma primarily involving dissociation or severe instability.
Importantly, trauma involving psychosis, severe dissociation, or unmanaged bipolar disorder is generally considered unsuitable for psychedelic interventions.
How Psilocybin Works in the Context of Trauma
Psilocybin affects the brain primarily through serotonin 2A receptors. Activation of these receptors leads to temporary changes in perception, cognition, and emotional processing.
One key mechanism is increased neuroplasticity. Psilocybin appears to temporarily loosen entrenched neural patterns, making the brain more adaptable and receptive to new perspectives. This can reduce the dominance of rigid fear-based networks that often sustain trauma symptoms.
Another important effect is enhanced emotional access. Individuals frequently report an increased ability to approach difficult emotions without becoming overwhelmed. This may support memory reconsolidation, a process in which traumatic memories are revisited and re-stored in a less threatening form.
Meaning-making also plays a central role. Psilocybin experiences often involve a reorganization of personal narratives, allowing individuals to reinterpret traumatic events within a broader, more compassionate framework.
What the Research Says About Psilocybin and Trauma
Direct clinical research on psilocybin for PTSD is still limited. Most large trials have focused on MDMA-assisted therapy for PTSD, while psilocybin studies have targeted depression, end-of-life anxiety, and addiction.
However, indirect evidence is relevant. Studies on treatment-resistant depression consistently show rapid and sustained symptom reduction following guided psilocybin sessions. Depression and trauma frequently overlap, particularly in emotional avoidance and negative self-concept.
Research on end-of-life anxiety demonstrates reduced fear, increased acceptance, and long-term shifts in meaning and emotional openness. Addiction studies suggest that psilocybin may help disrupt compulsive patterns and increase psychological flexibility.
Limitations remain significant. Sample sizes are small, protocols vary, and long-term outcomes are still being studied. Psilocybin is not a standardized trauma treatment, and outcomes are not predictable.
The evidence is promising, but it is not definitive.
Psilocybin-Assisted Therapy Explained
In research settings, psilocybin is never used in isolation. It is embedded within a structured therapeutic process.
The preparation phase focuses on building trust, clarifying intentions, and establishing psychological safety. Individuals learn what to expect and explore personal themes related to trauma.
The guided session takes place in a controlled environment with trained facilitators. Attention is given to emotional support, not direction or interpretation during the experience itself.
The integration phase is often the most important. Insights, emotions, and memories that emerge are explored and translated into daily life. Without integration, experiences may remain confusing or destabilizing.
This is why context and guidance matter more than the substance alone.
Microdosing vs Macrodosing for Trauma
Microdosing refers to taking very small amounts of psilocybin that do not produce perceptual changes. It is often discussed as a way to improve mood or focus.
Macrodosing involves doses that produce a full psychedelic experience and is the approach used in clinical research.
Evidence for microdosing in trauma is largely anecdotal. While some individuals report subtle benefits, microdosing does not reliably access traumatic material or support deep emotional processing.
Trauma work typically requires more than incremental mood changes. It involves engaging with deeply embedded fear and memory patterns, which is why therapeutic models focus on guided macrodosing rather than microdosing alone.
You might also like: Psychedelic Therapy: How Magic Truffles Are Used in Guided Sessions
Potential Benefits Reported by Participants
Participants in studies and therapeutic settings frequently report reduced avoidance and emotional numbing. Many describe increased self-compassion and a greater ability to face difficult memories.
Others report reframing traumatic experiences, seeing them as part of a larger life narrative rather than defining events. Improvements in emotional regulation and interpersonal openness are also commonly described.
Outcomes vary widely. Not everyone benefits, and effects depend heavily on preparation, support, and personal context.
Risks, Contraindications, and Psychological Safety
Psilocybin can intensify emotions and memories. Without adequate support, this can lead to re-traumatization rather than healing.
It is not suitable for everyone. Individuals with a history of psychosis, bipolar disorder, or severe dissociation face increased risks. Screening and professional guidance are essential.
Psychological safety depends on preparation, environment, dosage, and integration. These factors cannot be separated from the experience itself.
Legal and Ethical Context
Psilocybin remains illegal in many countries, though regulations vary. Some regions allow research use, others tolerate retreats operating in legal gray areas.
Research settings, retreat models, and underground therapy differ significantly in oversight, training, and safety standards. Legal status does not guarantee effectiveness or ethical practice.
Anyone exploring this topic should distinguish carefully between scientific research and unregulated offerings.
Trauma Healing Is More Than a Single Experience
Psilocybin is not a miracle cure. Trauma healing typically involves ongoing therapy, nervous system regulation, supportive relationships, and lifestyle changes.
When used responsibly, psilocybin may act as a catalyst rather than a solution. It can open a window for insight and emotional processing, but long-term change depends on what follows.
For some people, healing from trauma requires more than insight alone. It requires safety, guidance, and the space to gently reconnect with the body and nervous system.
Essence retreats are designed with this in mind. They offer a carefully held environment where psilocybin is approached with intention, professional support, and deep respect for individual boundaries. For those who feel ready to explore this path, a retreat can provide the structure, preparation, and integration that trauma-informed work requires.
If you are curious whether this approach may be right for you, check our upcoming retreats.
Frequently Asked Questions About Psilocybin for Trauma
Can psilocybin help with trauma recovery?
Some evidence suggests it may support emotional processing and psychological flexibility, but it is not a standalone treatment and not suitable for everyone.
Is psilocybin helpful for dealing with PTSD?
Research is still emerging. While indirect evidence is promising, psilocybin is not yet an established PTSD treatment.
Can psilocybin replace therapy?
No. Therapeutic support and integration are essential for safety and lasting benefit.
How does psilocybin differ from antidepressants?
Antidepressants are taken daily and aim to stabilize mood. Psilocybin is used sparingly and aims to facilitate psychological insight and change.
What are current treatments for post-traumatic stress disorder?
Evidence-based treatments include trauma-focused psychotherapy, EMDR, somatic therapies, and in some cases medication.
Sources
- Clinical conceptualisation of PTSD in psilocybin treatment: disrupting a pre-determined and over-determined maladaptive interpretive framework
- The Safety And Tolerability Of Comp360 (Psilocybin) In Participants With Post-Traumatic Stress Disorder
- The Emergence of Psilocybin in Psychiatry and Neuroscience